Paul Alexander has faced numerous challenges throughout his life, starting from his birth in 1946. He endured one of the most severe polio outbreaks in US history, which saw nearly 58,000 cases, mostly affecting children.
‘The Man in the Iron Lung’, Who Spent 70 Years Inside An Iron Lung, Paul Alexander Iron Lung has died at the age of 78.
Paul Alexander, who spent 70 years confined to an iron lung, has passed away at the age of 78. Afflicted by polio at the tender age of six, he was nicknamed “Polio Paul.” The disease left him paralyzed from the neck down in 1952, necessitating the use of the 600-pound metallic contraption to facilitate his breathing. Following the onset of symptoms, he was swiftly taken to a hospital in Texas, awakening to find himself dependent on the mechanical lung for survival.

News of Paul Alexander’s passing was shared on his GoFundMe page on Tuesday (March 12). Christopher Ulmer, who established the page, reflected on Paul’s remarkable journey: “After battling polio in childhood, he spent more than 70 years confined to an iron lung. Yet, during this time, Paul managed to attend college, pursue a career in law, and even become a published author. His story resonated far and wide, inspiring countless individuals worldwide. Paul exemplified extraordinary resilience and will be fondly remembered as an exceptional role model.”
Read More: The issue that could cost Trump the 2024 campaign
Philip, Paul Alexander’s brother, conveyed his gratitude to everyone who contributed to his brother’s fundraiser, expressing how it enabled Paul to spend his final years without the burden of financial worries.
Born in 1946, Mr. Alexander confronted numerous hurdles throughout his life. He navigated through one of the most severe polio outbreaks in US history, which afflicted nearly 58,000 individuals, predominantly children.
As reported by the New York Post, the poliovirus had a profound impact on Mr. Alexander, necessitating the use of a breathing machine due to the severity of the disease’s effects.
Polio, also known as Poliomyelitis, is a crippling and potentially fatal illness caused by the poliovirus. This virus spreads through person-to-person contact and can invade the spinal cord, leading to paralysis. In Mr. Alexander’s case, the virus weakened him to the point where he required assistance to breathe.
The iron lung employs a technique called “frog breathing,” which uses the throat muscles to force air past the vocal cords, allowing the patient to swallow oxygen one mouthful at a time, pushing it down the throat and into the lungs.

Following an emergency tracheotomy, Mr. Alexander was placed inside an iron lung to aid his body in battling the devastating effects of the disease. From that point onward, he depended on the full-body iron lung apparatus for his survival.
The iron lung utilizes a method known as “frog breathing,” where the throat muscles are engaged to propel air past the vocal cords. This enables the patient to ingest oxygen in small increments, guiding it down the throat and into the lungs with each swallow.
What is an iron lung?
During the mid-20th century, polio outbreaks swept across Europe and North America, hitting a peak in the United States in 1952, with a staggering 57,628 cases reported in just one year.
One of the most terrifying aspects of polio was its ability to cause muscle paralysis. If the paralysis affected the muscles responsible for breathing, patients were at risk of not being able to breathe on their own, which could be fatal. To combat this, researchers turned to technology.
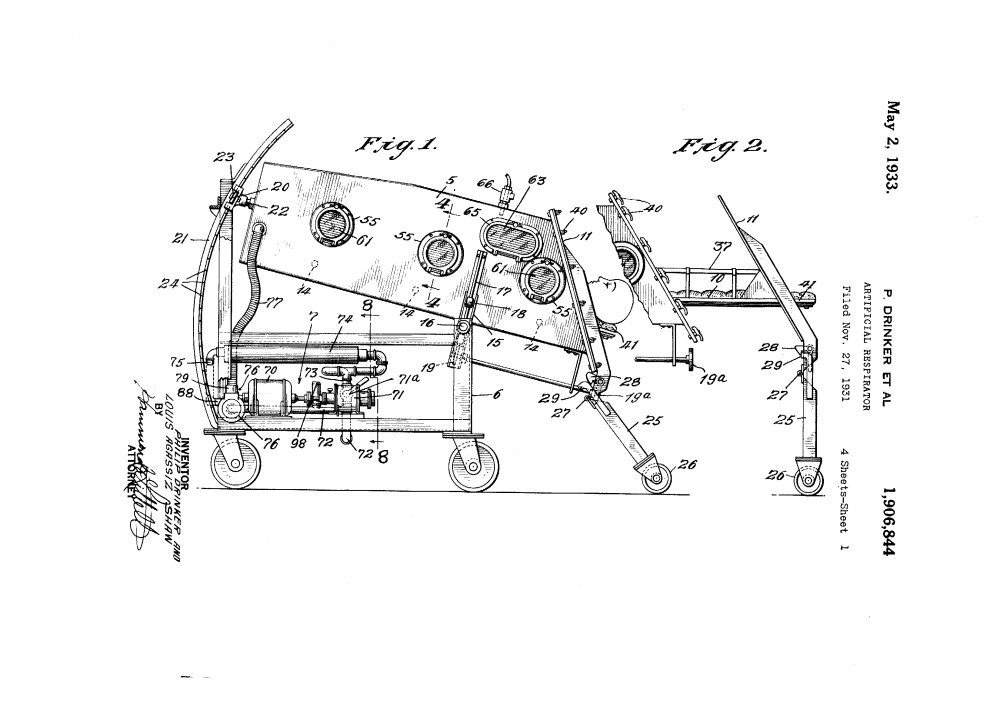
At Harvard University, a team developed a life-saving invention known as the “iron lung.” This device resembled a large metal box with bellows attached. Patients were placed inside the iron lung, and the bellows created a gentle suction that helped them breathe by expanding and contracting their chest.
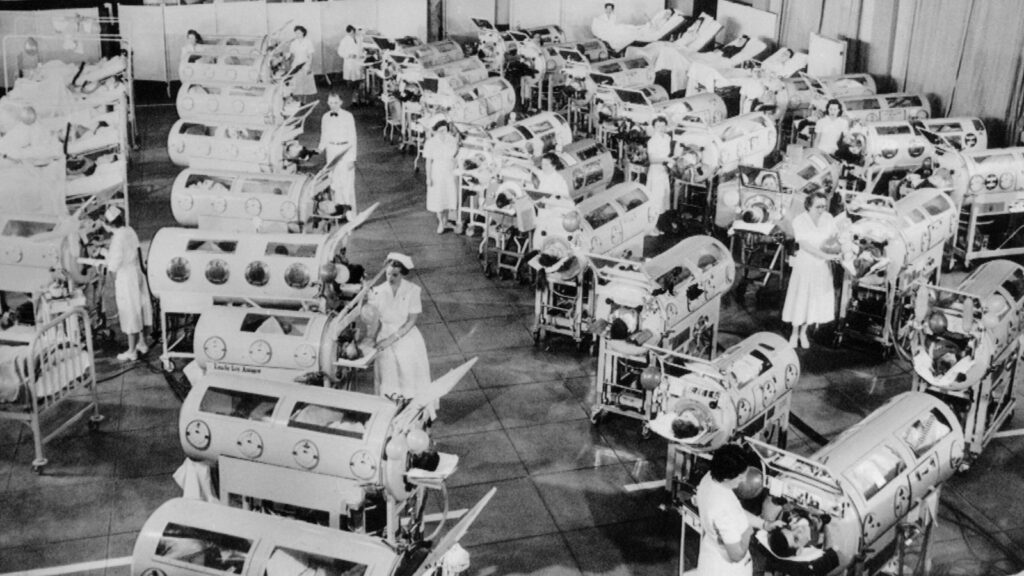
The iron lung quickly became a common sight in polio treatment centers during the mid-1900s. By 1939, approximately 1,000 iron lungs were in use across the USA, providing crucial support to patients who couldn’t breathe due to polio-induced paralysis. This innovation significantly improved the chances of survival for those affected by the disease.
How does an iron lung work?
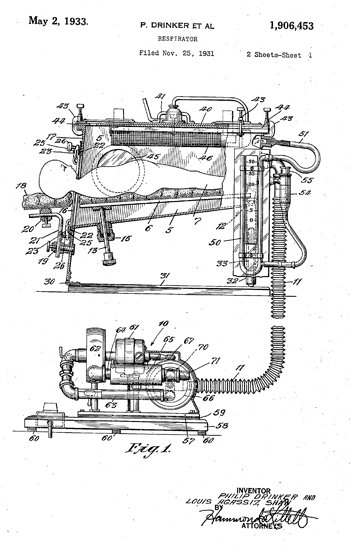
The respirator functioned by utilizing a method of artificial respiration known as External Negative Pressure Ventilation (ENPV).
The process involved the bellows withdrawing air from the sealed box in which the patient lay. As the air pressure inside the box decreased, the patient’s lungs naturally expanded, allowing fresh air to enter the diaphragm.
Conversely, when the bellows reintroduced air into the box, the increased air pressure caused the patient’s lungs to passively deflate, expelling air from them.
The rhythmic sound of air flowing in and out of the iron lung became a comforting reassurance, signifying the patients’ steady breathing.
What does an iron lung do?
Entering an iron lung was a disorienting experience for patients, many of whom were suffering from delirium and intense pain.
Life inside an iron lung posed significant challenges for both patients and caregivers. The array of tasks involved in caring for patients included administering blood transfusions, providing intravenous glucose feeds, inserting and replacing catheters, and making constant adjustments to both the patient’s body and the equipment.

In addition to medical care, caregivers attended to basic needs such as scratching itches, blowing noses, combing hair, washing bodies, and handling bedpans—all performed through the portholes whenever possible.
When the portholes were insufficient, essential tasks like physical therapy had to be completed within the brief periods when patients could breathe independently outside of the iron lung.
One of the biggest problems for patients was boredom. A mirror could be attached above the patient’s head, so they could see what was happening around them. They could also read books suspended in front of their faces if someone turned the pages for them.
In larger iron lung wards they had other patients nearby to provide companionship and psychological support but visiting hours for family were limited.